12 Strategies to Overcome Hashimoto’s Fatigue
Fatigue was the most debilitating symptom I experienced with Hashimoto’s. It started eight years before I was finally diagnosed in 2009, after I contracted mono (the Epstein-Barr virus) in college. I needed to sleep for 12 hours each night to be able to function, and by “function” I mean after hitting the snooze button on my alarm clock for two hours (ask my poor husband), I would drag myself out of bed and then had to drink 4-6 cups of caffeine everyday to keep myself awake. I often had Red Bull and Pepsi for breakfast and was the epitome of “wired but tired”.
I saw numerous doctors, and I was offered antidepressants, stimulant medications used for narcolepsy and ADHD, but no one thought to check my poor little thyroid. I then came across “chronic fatigue syndrome”, and was discouraged that there was “no cure”, so I slept half of my early twenties away thinking that I better just deal with it since no one could help me anyway.
When I was finally diagnosed with Hashimoto’s, part of me was relieved. I thought that I would finally get more energy. But this was not the case. Sure the thyroid medication helped; instead of sleeping for 12 hours, I only needed 11 hours of sleep after starting medications. But I didn’t give up. At the time of my diagnosis, I was working as a consultant pharmacist and had become accustomed to researching emerging healthcare information. Finding a way to get myself better became my mission.
It took me almost three years after my Hashimoto’s diagnosis to get my energy back, and I hope that some of the strategies that I used will help you get yours back too.
If you are dealing with Hashimoto’s fatigue, I’d like to share with you a few tips to get your energy back:
- The optimal TSH number for fatigue resolution
- The thyroid hormone that can block energy production
- The three types of fatigue-inducing anemia your doctor may miss
- The digestive enzyme that helped me reduce my sleep from 11 to 7 hours a night!
- A nutrient that can reverse thyroid fatigue in as little as 3 days
- An amino acid commonly deficient in people with thyroid conditions who take medications
- …plus much more!
My Strategies to Address Fatigue
1. The Importance of “Normal” TSH
Conventional endocrinologists often refer to the TSH test as the “gold standard” test for diagnosing and treating thyroid conditions. One major symptom of hypothyroidism is low energy. So, it’s important to make sure that your TSH is within the range of a healthy person without thyroid disease (not within the range of an elderly person or someone with subclinical thyroid disease).
TSH stands for Thyroid Stimulating Hormone, which is produced in the pituitary gland in your brain. The pituitary gland tells your thyroid to make and release thyroid hormones into your blood. A TSH test measures how much of this hormone is in your blood. In advanced cases of Hashimoto’s and primary hypothyroidism, this lab test will be elevated. (Read my post about interpreting your TSH test for more information). In the case of Graves’ disease and hyperthyroidism, the TSH will be low. Keep in mind, however, that people with Hashimoto’s and central hypothyroidism may have a normal reading on this test.
The National Academy of Clinical Biochemists indicates that 95 percent of individuals without thyroid disease have TSH concentrations below 2.5 μIU/mL. However, as of 2017, the official reference range for the TSH test in most labs in the U.S. runs from approximately 0.5 to 4.5 or 5.0 (μIU/mL). A patient with TSH levels within this range is considered to have normal thyroid function.
However, many labs have not adjusted that range in the reports they provide to physicians and have kept ranges as lax as 0.2-8.0 μIU/mL, and many physicians only look for values outside of the “normal” reference range provided by the labs and may not be familiar with the new guidelines. This is one reason why patients should always ask their physicians for a copy of their lab results. Despite some lab tests stating that a TSH of 8 or 5 μIU/mL is “normal”, most people feel best with a TSH between 0.5-2 μIU/mL.
In 2001, the results of the Basel Thyroid Study carried at the end of the 1990’s were published. Tiredness and fatigue remained as the cardinal impairment in hypothyroidism in spite of thyroid hormone therapy. An editorial in Thyroid, written by Peter Andreas Kopp in 2014, found that patients remain symptomatic (that is, they may experience symptoms like fatigue) despite having “normal” thyroid hormone levels.
Similar to the opinion of Kopp, Mary H. Samuels, a professor of the Oregon Clinical and Translational Research Institute, stated: “It is a common clinical observation that some otherwise healthy patients with hypothyroidism continue to complain of fatigue, poor mood, inability to concentrate, and vague cognitive difficulties (often described as ‘brain fog’) despite normal TSH levels.”
You may also be interested to know that of the 2,000+ people who took part in a survey I conducted, thyroid patients reported that optimizing their TSH helped improve their energy. Seventy-seven percent of my readers with a TSH level under 1 μIU/mL saw improvement in energy from medication interventions and 72 percent with TSH between 1 and 2 μIU/mL saw improvement in their energy levels.
From a personal perspective, I felt like a sloth when my TSH was within the “normal” range at 4 μIU/mL.
Read this article for more on TSH and how to talk to your doctor about TSH and adjusting your thyroid medications.
2. The Impact of Low T3/High Reverse T3
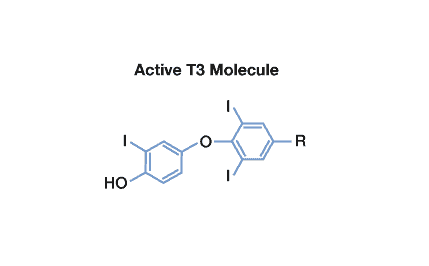
Triiodothyronine, or T3, is a hormone produced by the thyroid gland that is essential for keeping our metabolism going. T3 is the main “energy” hormone produced by the thyroid. When our cells see T3, they produce more energy, so it’s very important to ensure that we have adequate levels of active T3, as T3 tells our body to grow hair, boost metabolism, and create more energy.
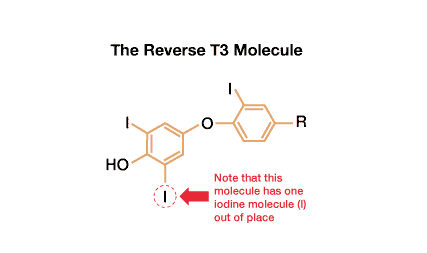
You’ll also want to avoid having a high level of reverse T3, which is a molecule related to T3 but blocks thyroid receptors in cells instead of activating them. When cells see this molecule, they slow down energy production.
Synthroid® or levothyroxine, a synthetic version of T4, is the most commonly prescribed thyroid medication, but only contains T4, a precursor to T3, our main “energy” hormone. T4 is converted to T3 in the body, but this doesn’t always happen due to numerous factors such as stress, nutrient deficiencies, and others, so we often continue to feel exhausted despite having normal T4 levels.
Factors that Inhibit T4 to T3 Conversion
| Stress | Medications | Aging | Surgery | Nutrient Depletions |
| Fasting | Chemotherapy | Diabetes | Soy | Growth Hormone Deficiency |
| Obesity | Goitrogens | Pesticides | Radiation | Low Progesterone |
| Iodine Excess | Heavy Metals | Cigarettes | Alcohol | Kidney and Liver Disease |
Ulta Labs is a great resource for ordering a free T3, free T4, and TSH test, as well as for checking your reverse T3 levels, online, without needing to get a thyroid lab request from your doctor. The lab also bills insurance (please check with your own insurance to make sure you qualify), and I love using it to get a discount on lab tests with my high-deductible insurance plan.If you continue to be fatigued while on medications, you can have your practitioner test your free T3 levels. (In some cases testing reverse T3 may also be helpful, although it’s not always necessary).
In the case that your T3 is low or in the bottom part of the reference range, or if you’re still symptomatic with T4 medications alone, you may benefit from adding a T3 containing medication such as Cytomel (liothyronine) to your current medication regimen, or switching to a T4/T3 combination medication such as WP Thyroid, Armour, Nature-Thyroid, or compounded T4/T3.
In my survey of over 2,000 readers, 76 percent reported improved energy with taking compounded T3/T4, 74 percent with taking Armour Thyroid, 74 percent with Cytomel, and 72 percent with Nature-Thyroid, while only 52 percent saw improved energy levels with Synthroid, the most commonly prescribed thyroid medication.
The takeaway from the survey showed that getting on the right thyroid medication helps many people get their energy back.
For further information, you can read my article about thyroid medications.
Also, be sure to download my FREE eBook on optimizing your thyroid medications!
3. Is Anemia Stealing Your Energy?
Many people think of iron deficiency as the cause of anemia, but there are actually three types of nutrient deficiencies that can lead to anemia that are common in people with Hashimoto’s – iron, B12, and folate.
Testing for Anemia
Your practitioner will usually run a blood test to check for hemoglobin and hematocrit to look for anemia. While helpful for advanced cases of anemia, this test may miss some subtle cases of anemia that can leave us feeling exhausted.
In addition to testing hemoglobin and hematocrit, I recommend testing ferritin, B12 and folate. Always be sure to get a copy of your lab tests. As with the “normal” range for TSH, the “normal” lab values for B12 and ferritin are often not optimal.
B12
Normal levels of Vitamin B12 are between 200-900 pg/mL, however, levels under 350 pg/mL are known to be associated with neurological symptoms. Furthermore, in my experience, you can have symptoms if your levels are below 700 pg/mL, and you may still benefit from a supplement.
In a study regarding the prevalence of Vitamin B12 deficiency among patients with thyroid dysfunction, it was found that autoimmune thyroid disease is also associated with the autoimmune disorder pernicious anemia, which may lead to malabsorption of Vitamin B12. The study concluded that in order to ensure proper treatment, Vitamin B12 screening is recommended upon initial diagnosis of autoimmune thyroid disease and then periodically thereafter.
As some people may have a difficult time absorbing B12 orally, B12 works best when taken as an injection or as a sublingual (under the tongue) drop.
Be sure to get the methylcobalamin or hydroxocobalamin version of B12 rather than a cyanocobalamin version of B12. These versions are better absorbed by most people.
I have found the liquid B12 5000 supplement by Pure Encapsulations to be very helpful for my clients. In my survey of 2232 of my readers with Hashimoto’s, 88 percent saw improvement in energy from B12 supplementation. You can read more about the thyroid and B12, as well as the optimal sublingual dosing regimen that can help you avoid shots.
Ferritin
Ferritin is the name given to your body’s iron reserve protein. “Normal” ferritin levels for women are between 12-150 ng/mL. However, the optimal ferritin level for thyroid function is between 90-110 ng/mL.
Ferritin is one of the most common deficiencies I see in people with Hashimoto’s, and in addition to fatigue, ferritin deficiency can also contribute to shortness of breath, restless leg syndrome, hair loss, insomnia, strange food cravings and mood swings.
While ferritin is likely to be deficient in up to 50 percent of women of childbearing age, as well as up to 80 percent of women who are pregnant or who are recently postpartum, I don’t recommend supplementing unless you’ve been tested to be deficient in ferritin. Too much iron/ferritin can also be a problem!
According to my survey, ferritin/iron supplementation improved energy levels for 82 percent of those who responded. While most iron supplements can cause digestive disturbances, two potential options may be better tolerated:
- OptiFerin-C contains ferritin and has helped many of my clients boost their ferritin levels. Calcium ascorbate, a natural, water soluble version of Vitamin C, is added to increase intestinal absorption.
- Thorne Iron Bisglycinate is an iron supplement that is more gentle on the stomach and less likely to cause constipation.
I recommend testing for ferritin before supplementing, and retesting your levels within 1-3 months, to ensure that you are supplementing enough (but not too much!).
If you’d like more details on some of the root causes of iron and ferritin deficiency as well as some advanced troubleshooting methods, you may want to read my article on Hair Loss.
Folate
Vitamin B9 is a necessary nutrient that naturally presents itself as folate, which plays a vital role in the formation of DNA and cell growth. In some cases, you may test normal or high for folate, but you could still be deficient in the right kind of folate for your body.
This is in the case of the MTHFR gene variation, which can impact how well your body metabolizes folate. Both folate and folic acid are forms of Vitamin B9, required for numerous critical bodily functions. However, folic acid is synthetic, while folate occurs naturally in foods such as broccoli, lamb, beets, and quinoa. Some people, including some individuals with Hashimoto’s, have a gene variation that prevents them from properly processing folic acid that may be present in less expensive supplements and processed foods. Some professionals claim this type of folic acid may even cause a build-up in the body, leading to toxicity.
Likewise, the MTHFR gene produces an enzyme necessary to process Vitamin B9 properly. This enzyme is also important for converting homocysteine to methionine, which the body needs for proper muscle growth and energy.
In addition to lifestyle changes, individuals with the MTHFR gene variation and high homocysteine levels may benefit from an activated or methylated version of folate, mainly because food alone does not provide sufficient levels. I have formulated Methylation Support, which contains all of the above-mentioned ingredients and may be helpful with reducing homocysteine levels to help people with the MTHFR gene variation.
Read more about MTHFR and Hashimoto’s.
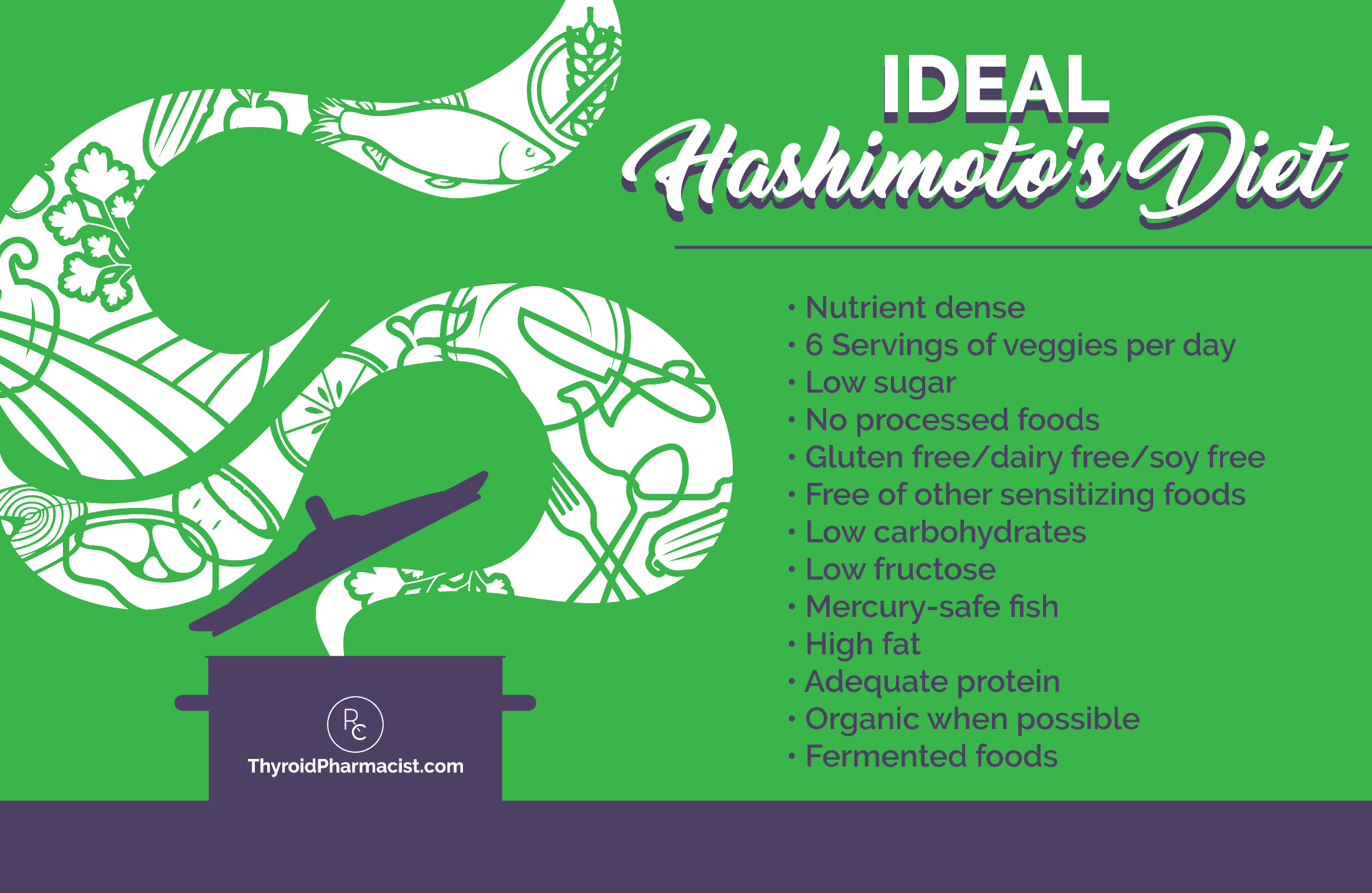
5. Discover Your Food Sensivities
Fatigue can be experienced from ingesting a food you are sensitive to. Food sensitivities are very different than food allergies, and many people are sensitive to specific food groups which can result in fatigue. People with Hashimoto’s often present with gluten, dairy, soy, egg, corn, and nut sensitivities. In fact, two of the most common food sensitivities found in people with Hashimoto’s are gluten and dairy.
(I know it can seem intimidating to cook or eat food without gluten and dairy, so I’ve created a 2-week Autoimmune Paleo recipe plan to get you started!)
Gluten is the main reactive protein found in wheat, and casein is the main reactive protein found in dairy. Growing evidence has shown that food sensitivities can negatively impact our bodies and trigger a wide range of symptoms, such as asthma, arthritis, mood disorders, and autoimmune disorders. My own clinical and personal experience has shown that non-Celiac gluten sensitivity is one of the biggest triggers in Hashimoto’s.
Changing my diet helped with fatigue, and I regained my energy. It also helped me eliminate bloating, symptoms of irritable bowel syndrome, anxiety, congestion, and carpal tunnel!
In my outcomes survey of people with Hashimoto’s, 75 percent reported improvement in energy from the Autoimmune Paleo Diet, and another 78 percent saw improvement in energy from the Paleo diet.
Food sensitivity testing may be helpful in some cases, but may not be affordable for many people. Not all tests are created equally, I have found the food sensitivity testing through Alletess to be the most accurate. The company offers food sensitivity testing (96 and 184 food panels) for people to self-order. I started with the 96 food panel, which was enough to pinpoint most of my food triggers, and I now repeat the 184 food panel on an annual basis to be sure that I’m staying on top of potential triggers, as our food sensitivities and reactions to foods tend to change with time.
You can also read more about food sensitivities and Hashimoto’s.
6. Balance Your Blood Sugar
Blood sugar imbalances can wreak havoc on our energy levels as well as cause anxiety. People with blood sugar imbalances will often have times of the day where they feel especially tired, weak and/or anxious, such as “morning fatigue” or the “afternoon slump”.
That’s why balancing blood sugar levels should be one of the priorities for anyone who is hoping to overcome fatigue. Balancing my blood sugar made a big difference for me, helping me feel more energetically balanced and less anxious throughout the day. As a side bonus, most people with Hashimoto’s will find that their thyroid antibody levels will drop thanks to balancing their blood sugar!
Before I balanced my blood sugar, I would get “hangry” (hungry + angry) multiple times per day. I found that the high carbohydrate foods I was eating were causing huge blood sugar swings, and I didn’t realize these swings were causing a spike in my thyroid antibodies and weakening my adrenals.
Practitioners, like myself, who focus on reversing Hashimoto’s, often describe blood sugar imbalances as adding fuel to the fire in autoimmune thyroid disease. I wasn’t aware that I had blood sugar issues when I was first diagnosed (despite being a self-admitted sugar addict).
Researchers in Poland found that up to 50 percent of patients with Hashimoto’s have an impaired tolerance to refined or simple carbohydrates like processed sugar or refined grains that have had the nutrients removed. This means that after consuming carbohydrate-rich foods, their blood sugar goes up too high, too quickly, which leads to a rapid, and often extreme release of insulin. These insulin surges can cause low blood sugar (reactive hypoglycemia), which in turn can cause troublesome symptoms like lightheadedness, nervousness, anxiety, and fatigue.
However, eating a low glycemic index diet can help you feel fuller longer. It can also improve cholesterol and blood sugar levels, enhance cognitive performance, improve energy, and reduce acne. The diet can also lower your risk of developing diabetes, heart disease, some cancers, and can promote weight loss as well.
I recommend these blood sugar rules to help you feel better.
7. Enhance and Optimize Digestion
The digestive process is an energy intensive one. Studies have shown that people with Hashimoto’s and hypothyroidism often do not have adequate levels of stomach acid, some don’t produce ANY stomach acid, making protein digestion inefficient and even more draining of our energy.
Discovering that I had a deficiency of stomach acid was a huge “aha” moment for me! I couldn’t believe how energetic I became when I started taking Betaine with Pepsin with my protein containing meals.
My 10-year long debilitating fatigue was lifted practically overnight, and I went from sleeping for 11-12 hours per night to 8 hours — just because I started digesting my foods better. I felt like Bradley Cooper in Limitless after I started taking Betaine with Pepsin! Finally having enough energy gave me the confidence that I could overcome Hashimoto’s and my long list of health struggles. It even helped with my brain fog, and I was able to come up with all kinds of clever words much quicker. My humor came back.
I started writing my book about overcoming Hashimoto’s the morning after I took the dose of Betaine with Pepsin. The restored energy gave me hope that I would be able to devote myself to research and find the root cause of my condition, then share that knowledge to help others.
Betaine with Pepsin promotes healthy digestion and supports nutrient absorption, such a protein, calcium, Vitamin B12, and iron. I have found it very beneficial for anyone seeking enhanced digestive function.
Out of 627 of my readers who took Betaine HCI and Pepsin, 59 percent said it made them feel better and saw improved energy levels, 33 percent said it make them feel worse, while 7 percent saw no difference in their symptoms. These results lead me to estimate that 50-70 percent of people with Hashimoto’s are likely to have a deficiency in stomach acid, and the 33 percent of those who felt worse were likely not deficient in stomach acid. Those who did not see any improvement may not have been dosed adequately, as the dosage of Betaine with Pepsin should be individualized.
If you have a thyroid condition and continue to struggle with fatigue, you can download my Low Stomach Acid Quick Start Guide.
Learn How to Beat Fatigue with Betaine

Find out if the supplement that helped lift me from 10 years of debilitating fatigue can reduce your fatigue too! I'll teach you the right way to use it, plus alternative ways to support stomach acid if this supplement is not for you.
8. Sunshine Deficiency
A lack of sunshine can lead to fatigue, due to two very specific reasons, vitamin D deficiency and light deficiency.
Low levels of vitamin D can be associated with fatigue, hypothyroidism, and autoimmunity in general. We can get vitamin D from sunshine, certain foods, and supplements, but it’s not always easy to ensure you are getting enough. Your goal should be to get your vitamin D levels between 60-80 ng/dl. This is especially true for those who have a history of contracting the Epstein-Barr virus (EBV).
Vitamin D deficiency is more commonly found in people with Hashimoto’s—68 percent of my readers with Hashimoto’s reported also being diagnosed with vitamin D deficiency, and 67 percent saw improvement in energy from increasing their vitamin D levels. Research done in Turkey found that 92 percent of Hashimoto’s patients were deficient in vitamin D, and another 2013 study found that low vitamin D levels were associated with higher thyroid antibodies and worse disease prognosis.
I’ve personally found that most of my clients who are in remission from Hashimoto’s keep their levels of vitamin D between 60-80 ng/mL.
My #1 recommendation for addressing both of these deficiencies is a beach vacation. (Please print this and show it to your boss or spouse whenever necessary—I know I have to remind my husband every winter :-)). But if you can’t get to the beach just yet, the recommendations below should work even in the darkest and coldest of winters!
Who is at Risk for Vitamin D Deficiency?
Pretty much anyone who is not a full-time lifeguard in Southern California is at risk of being deficient in Vitamin D. Vitamin D deficiency is rampant—very common in most North Americans, Europeans, and Australians—and affects a large number of people with Hashimoto’s. A low-fat diet or fat malabsorption increases the risk. The best way to restore optimal Vitamin D levels is through sun exposure, safe tanning beds, and an oral vitamin D3 supplement. The secondary best sources of vitamin D are from foods like wild salmon and cod liver oil.
Vitamin D advocates recommend 15 minutes of unexposed skin without sunscreen around noon. Perhaps you can go for a walk during lunchtime? If you are fair skinned and not used to the sun, you may need to start a bit slower. Be careful not to overexpose yourself to prevent getting a sunburn.
I also recommend Blue Light Therapy Boxes. Clinically proven to boost energy and mood naturally, as well as fight the winter blues, blue light therapy boxes allow you to get the light you need wherever you live or work. It may take a week or so before you begin to feel your energy return, and you will want to use it daily for at least 30 minutes to see the best results.
I generally recommend using the box first thing in the morning as you’re getting ready for work, as well as in the early afternoon to give yourself another energy boost. I don’t recommend using the light too close to bedtime, unless you’re planning to stay up late!
I have personally used this type of light preventatively during cloudy weather as well as whenever I feel like I need an energy boost and can’t get outside or to the beach.
9. Is Adrenal Fatigue Getting You Down?
Adrenal fatigue can make you feel like you are dragging around 50 pounds of concrete, especially in the later phases of adrenal fatigue when your cortisol becomes depleted. Adrenal fatigue is one of the major reasons we feel exhausted despite taking thyroid medications.
With optimal adrenal function, in the morning, cortisol spikes, giving you a natural jolt to get you out of bed. Those in advanced levels of adrenal fatigue won’t make enough cortisol in the morning and may find themselves having difficulty with getting up in the morning and sustaining good energy throughout the day. A common pattern I often see is “the afternoon person”, or someone who struggles in the morning and in the evening and has just a few good hours in the afternoon, or the “tired night owl”, a person who feels tired most of the day then gets a second wind at bedtime when the day’s cortisol is released.
Without sufficient cortisol levels, we may become dependent on caffeine… Caffeine boosts cortisol levels temporarily, but does weaken the adrenals in the long term. In fact, drinking too much caffeine can create a vicious cycle of unrestful sleep/fatigue/needing more caffeine. Getting adequate sleep as well as weaning off caffeine (notice, I didn’t say stopping cold turkey) can help with rebalancing the adrenals.
Try hot lemon water first thing in the morning instead. It’s a great substitute for caffeine and helps to provide relief from fatigue.
 I have found that the ABC’s can be incredibly helpful for supporting the adrenals and energy levels.
I have found that the ABC’s can be incredibly helpful for supporting the adrenals and energy levels.
A- Adrenal Adaptogens
B- B vitamins
C- Vitamin C
B- B vitamins
C- Vitamin C
I created Adrenal Support from Rootcology, which contains a blend of the ABC’s. You should see improvements in your energy levels and resilience within a few days of starting Adrenal Support.
In some cases, additional adrenal testing and protocols may be indicated. I cover these in great depth in Hashimoto’s: The Root Cause, and Hashimoto’s Protocol.
You can also learn more about the thyroid and adrenals here.
10. Is Your Liver Congested?
The liver’s function is to remove toxins from our bodies. These toxins can come from various external sources, such as molds, or from internal sources like an imbalance of gut bacteria or pathogens. Some of us may be exhausted because we cannot process the toxins that are present in our bodies. The toxins saturate our liver enzymes, making us feel fatigued.
Some of the most common toxins in the environment include:
- Pesticides
- Herbicides
- Heavy metals
- Food additives
- Formaldehyde
- Solvents/cleaning materials
It’s a good idea to reduce your exposure to toxins in your environment. A few ideas include the use of an air purifier, drinking filtered water, stopping the use of cosmetics that contain petrochemicals, avoiding preservatives and additives, stopping the use of harsh cleaning agents and aerosols, and eliminating molds in your home.
 I have also found N-Acetyl-Cysteine, a supplement that supports liver detox capabilities, to be worth considering.
I have also found N-Acetyl-Cysteine, a supplement that supports liver detox capabilities, to be worth considering.
I have a whole chapter on detoxification in my book, Hashimoto’s: The Root Cause and I cover liver support in great detail in my new book Hashimoto’s Protocol.
You can also read about how supporting the liver is key to recovering from thyroid disease. You’ll find signs and causes of toxic overload, how liver impairment is related to Hashimoto’s, who is most at risk, and so much more.
11. Boost Thiamine and Boost Your Energy
Studies have found that people with Hashimoto’s are often deficient in the B vitamin, thiamine (Vitamin B1).
Thiamine is essential for energy production and carbohydrate digestion. Our bodies need thiamine to make adenosine triphosphate (ATP), which our cells use for energy, and it plays a key role in supporting the nervous system. B1 is thought to strengthen the immune system and help our bodies withstand stressful situations. But, in order to absorb enough thiamine into our bodies, we also need adequate supplies of B6, B12, and folate.
 What’s really exciting is that taking 600 mg per day can restore energy levels in as little as three days! That’s great news for someone who suffers from fatigue. I have written about the thyroid/thiamine connection in my blog posts, and I still get hugs from people I meet at conferences who have reported that thiamine has changed their lives.
What’s really exciting is that taking 600 mg per day can restore energy levels in as little as three days! That’s great news for someone who suffers from fatigue. I have written about the thyroid/thiamine connection in my blog posts, and I still get hugs from people I meet at conferences who have reported that thiamine has changed their lives. 
I recommend Benfomax from Pure Encapsulations for best results. It is non-GMO, gluten free and vegan. It’s one of the highest quality thiamine supplements on the market. Please read more about the thiamine and thyroid connection.
12. L-Carnitine for Thyroid Fatigue
L-carnitine is an amino acid that is naturally produced in the body. It helps transport fatty acids into the mitochondria where they can be burned up and used as fuel.
L-carnitine levels may be decreased in hypothyroidism, potentially due to reduced synthesis of L-carnitine while we are in a hypothyroid state. Taking a thyroid medication can boost the production of L-carnitine, but it can also work as a vacuum, taking the L-carnitine from the body and resulting in an overall deficiency of it.
The results of a recent study regarding L-carnitine supplementation for the management of fatigue in patients with hypothyroidism found that L-carnitine may be useful in alleviating fatigue symptoms in hypothyroid patients, especially in those younger than 50 and those who have hypothyroidism due to a thyroidectomy.
In the study, 60 patients who were experiencing fatigue were given L-carnitine for 12 weeks. A dose of 1,980 mg was given to 30 people who were taking thyroid hormones (either due to Hashimoto’s or post-thyroidectomy), while 30 people received a placebo.
 After 12 weeks, the researchers noted that the group receiving L-carnitine did indeed show improvements in fatigue, with the most significant improvements seen in “brain fatigue.”
After 12 weeks, the researchers noted that the group receiving L-carnitine did indeed show improvements in fatigue, with the most significant improvements seen in “brain fatigue.”
I have personally seen people “awaken” with the use of L-carnitine.
A dose of two capsules twice a day, or 2,000 mg of L-carnitine is recommended.
The Takeaway
Many people endure the exhausting symptoms of fatigue every day. I know first hand how tiredness and fatigue can impact everyday life and leave you exhausted. Overcoming Hashimoto’s fatigue is an important step in regaining your energy and getting on with life, and the interventions listed above may help with that. You have the power to take back your health.
If you’re looking for more tips, I have a FREE ebook that includes a summary of the most helpful strategies to overcome fatigue in a simple and easy to read format, including some of the supplements that will make a difference right away. Sign up below to join my mailing list and download my eBook: Overcoming Thyroid Fatigue.
I hope that you can get your energy back soon! 

P.S. You can also download a free Thyroid Diet Guide, 10 Thyroid friendly recipes, and the Nutrient Depletions and Digestion chapter. You will also receive occasional updates about new research, resources, giveaways and helpful information.
For future updates, make sure to follow us on Facebook!
References
- Brownstein D. Overcoming Thyroid Disorders. West Bloomfield, MI: Medical Alternatives Press; 2008.
- Arakawa, Y. Association of polymorphisms in DNMT1, DNMT3A, DNMT3B, MTHFR and MTRR genes with global DNA methylation levels and prognosis of autoimmune thyroid disease. Clinical and Experimental Immunology. 170:194–201.
- Tejani AM, Wasdell M, Spiwak R, Rowell G, Nathwani S. Carnitine for fatigue in multiple sclerosis. Cochrane Database of Systematic Reviews. 2012;5. DOI: 10.1002/14651858.CD007280.pub3.
- Tomassini V, Pozzilli C, Onesti E, Pasqualetti P, Marinelli F, Pisani A, et al. Comparison of the effects of acetyl L- carnitine and amantadine for the treatment of fatigue in multiple sclerosis: results of a pilot, randomised, double- blind, crossover trial. Journal Neurological Sciences. 2004; 218(1-2):103–8.
- Lloyd AR. Hales JP. Gandevia SC: Muscle strength, endurance and recovery in the post-infection fatigue syndrome. J Neurol Neurosurg Psychiatry. 1988;51:1316-1322.
- Kuratsune H. Yamaguti K, Takahashi M. et al. Acylcamitine deficiency in Chronic Fatigue Syndrome. Clin infect Dis. 1994;1:S62-67.
- Chiba S, Ito M, Matsumoto H. Amantadine treatment for refractory pain in patients with multiple sclerosis. Can J Neurol Sci. 1992;19:309.
- Murray TJ. Amantadine therapy for fatigue in multiple sclerosis. Can J Neurol Sci. 1985;12:251-254.
- Rosenberg GA. Appcnzcller O. Amantadine, fatigue and multiple sclerosis. Can J Neurol Sci.1988;45:1104-1106.
- Fukuda K, Strauss SE, Hickie I, et al. The Chronic Fatigue Syndrome: A comprehensive approach to its definition and study. Ann Intern Med. 1994;121:953-959.
- An JH, Kim YJ, Kim SH, et al. L-carnitine supplementation for the management of fatigue in patients with hypothyroidism on levothyroxine treatment: a randomized, double-blind, placebo-controlled trial. Endocr J. 2016;63(10):885-895.
- Collins AB, Pawlak R. Prevalence of vitamin B-12 deficiency among patients with thyroid dysfunction. Asia Pac J Clin Nutr. 2016;25(2):221-6. doi: 10.6133/apjcn.2016.25.2.22.
- Meier C. TSH-controlled L-thyroxine therapy reduces cholesterol levels and clinical symptoms in subclinical hypothyroidism: a double blind, placebo-controlled trial (Basel Thyroid Study) J. Clin. Endocrinol. 2001;86:4860–4866.
- Zulewski H. Estimation of tissue hypothyroidism by a new clinical score: evaluation of patients with various grades of hypothyroidism and controls. J. Clin. Endocrinol. 1997;82:771–776.
- Meier C. Serum thyroid stimulating hormone in assessment of severity of tissue hypothyroidism in patients with overt primary thyroid failure: cross sectional survey. BMJ. 2003;326:311–312.
- Winther KH. Disease-specific as well as generic quality of life is widely impacted in autoimmune hypothyroidism and improves during the first six months of levothyroxine therapy. PLoS One. 2016;11.
- Kopp P.A. Commentary on: guidelines for the treatment of hypothyroidism. Thyroid. 2014;24:1667–1669.
- Samuels MH. Effect of thyroid function variations within the laboratory reference range on health status, mood, and cognition in levothyroxine-treated subjects. Thyroid. 2016;26:1173–1184.
- Saravanan P. Psychological well-being in patients on ‘adequate’ doses of l-thyroxine: results of a large, controlled community-based questionnaire study. Clin. Endocrinol. 2002;57:577–585.
- Wekking E.M. Cognitive functioning and well-being in euthyroid patients on thyroxine replacement therapy for primary hypothyroidism. Eur. J. Endocrinol. 2005;153:747–753.
- Walsh J.P. Small changes in thyroxine dosage do not produce measurable changes in hypothyroid symptoms, well-being, or quality of life: results of a double-blind, randomized clinical trial. J. Clin. Endocrinol. 2006;91:2624–2630.
- WebMD. L-CARNITINE: Uses, Side Effects, Interactions and Warnings. WebMD. https://www.webmd.com/vitamins-supplements/ingredientmono-1026-L-CARNITINE.aspx. Accessed March 2, 2018.
- Billewicz WZ. Statistical methods applied to the diagnosis of hypothyroidism. Q. J. Med. 1969;38:255–266.
Note: Originally published in May 2015, this article has been revised and updated for accuracy and thoroughness.

No comments:
Post a Comment