What Happens In Your Body When You Suffer From Thyroid Disease?
August 9th, 2017
Contributing writer for Wake Up World
Have you ever wondered how can the thyroid, such a small butterfly shaped gland be responsible of so many negative symptoms that affect your entire metabolism? This happens because the thyroid functions are interconnected with each system in the organism. If the thyroid doesn’t work well, neither do you and you can’t possibly feel well.
Thyroid disease has been on the rise for the past few decades, yet many thyroid dysfunctions are not correctly diagnosed or are diagnosed too late. The thyroid hormone is found in each cell of your body and this is a major reason many experts believe the conventional way of diagnosing thyroid illnesses is not precise: measuring TSH (thyroid stimulating hormone) exclusively from blood doesn’t reflect the intracellular level of the hormone. Additionally, the thyroid gland and the hormones it is utilizing don’t exist in isolation inside the organism. This is why it is necessary to evaluate the functional relationships between the thyroid and various other organs, glands and systems.
The Digestive System.
Chronic constipation is a common symptom when dealing with hypothyroidism. Thyroid dysfunction slows down the food transport in the intestines. This raises the risk for infections with pathogens in the intestines, contributes to inflammation, malabsorption and food sensitivities. The low level of gastrin determines intestinal discomfort, reflux, bloating and the low level of gastric acid determines protein deficiency.
Thyroid hormones strongly influence the tight junctions in the stomach and small intestine, which form the impermeable barrier of the digestive system. Leaky gut syndrome is a primary factor in autoimmune diseases as Hashimoto.
Studies have shown that thyroid hormones T3 and T4 protect the intestinal mucosal barrier against stress induced ulcer development. Inflammation in the digestive system reduces T3 through raising cortisol levels. Additionally, intestinal bacteria assists in transforming 20 percent of inactive T4 hormone into its active T3 form. Intestinal dysbiosis – the imbalance between pathogenic and beneficial intestinal flora, drastically reduces this conversion.
The Gallbladder and Liver.
Hypothyroidism affects the gallbladder function through reducing bile flow. The liver metabolizes hormones, filters toxins and cleans the blood. Hypothyroidism interferes with this process and the gallbladder and liver become congested, leading to gallstones. Thyroid hormones affect the most the liver cells responsible for detoxification. At the same time, liver dysfunction will affect both thyroid function, as well as the detoxifying mechanisms of the body. A low T3 level usually reflects liver dysfunction, because the T4 – T3 conversion takes place in the liver. This can also be confirmed through analyzing liver enzymes GGTP and ALT and their high level.
The Bone System.
The thyroid gland produces and stores calcitonin, a regulatory hormone of calcium. Hypothyroidism interferes with the correct process of long bones formation.
Insulin and Blood Sugar.
Persons with a reduced thyroid function absorb glucose slower than normal and so the cells can’t use it to produce energy. The surge of insulin produced in the insulin resistance stage accelerates the thyroid destruction in people with autoimmune thyroid disease. When the gland is destroyed, the hormone production will lower.
When the blood sugar level sinks below normal (hypoglycemia), the adrenal gland responds by secreting cortisol. This transmits to the liver to produce more glucose in order to reestablish normal levels. Unfortunately for the hypoglycemics, the constant cortisol production determined by hypoglycemic episodes suppress the pituitary gland function. This also negatively affects the thyroid.
Estrogen and Progesterone.
Estrogen must first be transformed in a water soluble state in the liver in order to be eliminated from the body. During this process estradiol is made, a secondary type of estrogen. Hypothyroidism can block this process, contributing to estrogen dominance, breast cancer, uterine fibroids and ovarian cysts.
Thyroid hormones sensitize the body’s cells so that they can be available to progesterone. When receptors are not exposed to enough thyroid hormones, they loose their ability to allow progesterone to enter the cells.
Fat Burning.
Hypothyroidism slows down the body’s metabolism and its ability to burn fat. Adrenal hormones that stimulate fat burning are not efficient anymore and the cells’ receptors that answer to lipase – an enzyme which metabolizes fat, are not available.
Cholesterol.
Cholesterol is the main source for steroid hormones formation. Cell absorption of LDL cholesterol will be reduced if there isn’t sufficient thyroid hormone in the cells. LDL will raise significantly in blood due to dysfunctional utilization of thyroid hormone. When the thyroid of a person is underworking, fat will be stored much faster than the body can burn it, which will determine high triglycerides and LDL cholesterol in blood.
Adrenal Glands.
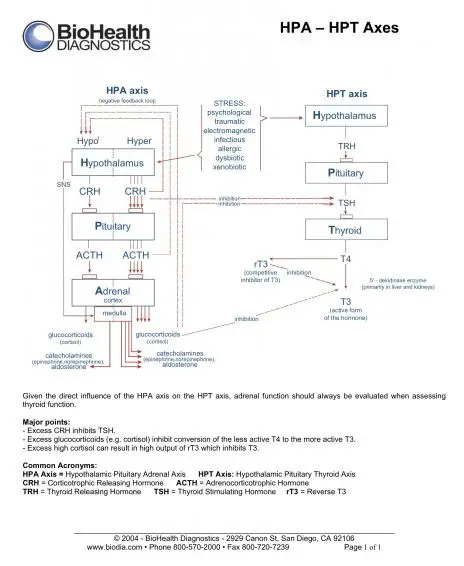
The HPT axis (hypothalamus – pituitary – thyroid) works as a feedback loop; if the thyroid is functioning well, your cells have sufficient energy. Some dysfunctions which can be involved in the imbalance of the axis are: methylation cycle dysfunction, dysfunction of the HPA axis (hypothalamus-pituitary-adrenal), nutrient deficiencies which are needed for thyroid hormone formation (selenium, zinc, iron, gluthatione, vitamin A, D, iodine) and liver dysfunctions.
Adrenal glands fall under the control of the sympathetic nervous system. The thyroid is strongly influenced by the parasympathetic nervous system. Often a person with hypothyroidism is in a dominant parasympathetic state, and so the sympathetic system is weaker. Considering the strong relation between adrenals, hypothalamus and thyroid, one can observe how the dysfunctional state of the exhausted adrenal glands can cause a cascade of problems for thyroid function.
As you can see in the below figure, glucorticoid hormones (which include cortisol) can suppress T4 – T3 conversion. So a person with a high level of cortisol (and stress) risks to suffer from low thyroid function. Additionally, the high cortisol level can result in excessive production of inactive reverse T3 (rT3), which will compete with T3 and so suppress thyroid function.
Other stress hormones like CRH produced by the hypothalamus will have an inhibitory effect on the thyroid, blocking TSH transport to the thyroid.
On top of this, if a person presents mercury toxicity and doesn’t consume a clean and correct diet for her/his metabolism, the risk of developing hypothyroidism will become even higher.
References:
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1856434/?tool=pubmed
- http://www.ncbi.nlm.nih.gov/pubmed/12269922
- http://www.ncbi.nlm.nih.gov/pubmed/1555538
- http://www.ncbi.nlm.nih.gov/pubmed/18506897
- http://www.ncbi.nlm.nih.gov/pubmed/12660641
- http://www.ncbi.nlm.nih.gov/pubmed/18506897
- http://onlinelibrary.wiley.com/doi/10.1111/j.0954-6820.1969.tb01517.x/abstract
No comments:
Post a Comment